Breast Cancer: Stages
The way in which a cancer spread or grow is called staging.
Staging basically describes the location of cancer, the extent of growth of
cancer, and area of spreading of cancer. The stage of cancer is confirmed by
diagnostic tests. The confirmation of staging helps the doctor to decide the
best kind of treatment and can predict prognosis of a patient, which are
chances of recovery. Different types of cancer have different stage
description.
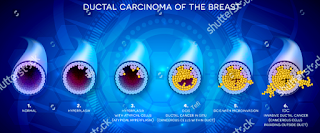 |
| Stages of ductal carcinoma of breast cancer |
TNM staging system
The commonly used tool to describe the stages of cancer is the TNM
system. Doctors take the results from diagnostic tests and employ them to find
the answer of following questions:
·
Tumor (T): How
large is the extent of primary tumor? Where is it’s location?
·
Node (N): Has
the tumor grow to the lymph nodes? If yes, where and how many?
·
Metastasis (M): Has
the cancer spread to certain other parts of the body? If yes, where and how
much?
The stages of cancer for each person are determined from the
combined results.
There are mainly five type of stages: A stage which is
non-invasive ductile carcinoma in situ (DCIS) is called stage 0 (zero). The
other stages from I through V are employed for invasive breast cancer.
Staging can be pathological or clinical. Pathological surgery is
based on removing breast tissue and lymph nodes during surgery. The results are
usually obtained after many days after surgery. Generally, pathological staging
gives the complete information for determining prognosis of a patient. While
clinical staging depends on results of tests before surgery which may include
mammogram, MRI scans, physical examination and ultrasound.
The further detail of the TNM system for the breast cancer is
given below:
Tumor (T)
Utilizing the TNM system, the “T” with a letter or number from 0
to 4 is used for describing the location and size of the tumor. The size of
tumor is measured in centimeter (cm). A centimeter is nearly equal to the width
of a standard pencil or pen.
Stages
may also be divided into further smaller groups in order to explain the more
detail of tumor. The information of specific stages of tumor are listed below:
TX: The primary tumor cannot be graded
T0 (T plus zero): This indicates no evidence
of cancer in the breast.
Tis: This
indicates to carcinoma in situ. The cancer is restricted within the ducts of
breast tissue and has not proliferate into the surrounding tissue of the
breast. Breast carcinoma in situ has 2 types.
·
Tis (DCIS): DCIS is noninvasive type of cancer, but it can develop into invasive
breast cancer later if it is not removed. DCIS refers to the situation where
cancer cells have been confined into ducts of breast and have not proliferate
past the layer of tissue where they began.
·
Tis (Paget’s): Paget’s disease of the nipple is a rare and early noninvasive form of
cancer that is present only in the skin cells of nipple. Paget’s disease
sometimes become associated with invasive breast cancer. If another invasive
breast cancer is present, it is classified depending on the stage of invasive
tumor.
T1: The
tumor in the breast at its widest area is 20 milli-meters or smaller in size.
Its size is little less than an inch. This stage is further divided into four
substages based on the size of the tumor:
·
T1mi is a tumor having size 1 mm or even smaller
·
T1a is a tumor having size larger than 1 mm but 5 mm or even smaller
·
T1b is a tumor having size larger than 5 mm but 10 mm or even smaller
·
T1c is a tumor having size larger than 10 mm but 20 mm or even smaller
T2: The
tumor having size larger than 20 mm but not larger than 50 mm.
T3: The tumor having size larger than 50 mm.
T4: The tumor falls into 1 of the groups given below:
·
T4a refers to the tumor that has grown into the chest wall.
·
T4b refers to the tumor that has grown into the skin.
·
T4c refers to the tumor that has grown into the chest wall and the
skin.
·
T4d is refers to inflammatory breast cancer.
Node (N)
The “N” in the TNM staging system refers for lymph nodes. Regional
lymph nodes include:
·
Lymph nodes that are lacated under the arm are termed as axillary
lymph nodes
·
Below and above the collarbone
·
Under the breastbone which is termed as internal mammary lymph
nodes
Lymph
nodes that are present in other parts of the body are termed as distant lymph
nodes. If the doctor diagnosis lymph nodes without surgery using various tests
and physical examination, the letter “N” is placed by “C” for clinical staging.
If the doctor diagnosis lymph nodes after surgery which is a more authentic
evaluation, the letter “N” is replaced by “P” for pathological staging. The
pathological staging is described by the following information.
NX: Refers to the lymph nodes were not evaluated.
N0: Either
of the following situations:
·
No cancer was diagnosed in the lymph nodes.
·
Lymph nodes contain areas of cancer that are smaller than 0.2
millimeter (mm).
N1: The
cancer has proliferated to 1 to 3 internal mammary lymph nodes and axillary
lymph nodes. If the size of tumor located in the lymph nodes is larger than 0.2
mm but equal to 2mm or smaller, it is termed as “micrometastatic” (N1mi).
N2: The
cancer has proliferate to 4 to 9 axillary lymph nodes. Or it has proliferate to
the internal mammary lymph nodes, but not found the axillary lymph nodes.
N3: The
cancer has proliferate to 10 or more axillary lymph nodes. Or it has
proliferate to the lymph nodes present under the collarbone or clavicle. It may
have also proliferate to the internal mammary lymph nodes. Tumor that has
proliferate to the lymph nodes above the clavicle is termed the supraclavicular
lymph nodes, is also described as N3.
If the tumor is present in the lymph nodes, it is important to
find the number of lymph nodes that are involved in cancer and also their
location to help the doctors to plan treatment. The pathologists can evaluate
the number of axillary lymph nodes that are involved in cancer after removing
them during surgery. If the cancer is located in axillary lymph nodes,
treatments other than surgery such as chemotherapy, radiation therapy and
hormonal therapy are used during early stages of treatment.
Metastasis (M)
The “M”
in the TNM system refers to whether has proliferated to various parts of the
body which is termed as distant metastasis. This is no longer falls into the
category of early-stage or locally advanced cancer.
MX: Refers to distant proliferation that cannot be evaluated.
M0: Refers
to the disease that has not metastasized.
M0 (i+): It
refers to the condition where no clinical or radiographic evidence of distant
metastases are evaluated. Microscopic evidences of cancer cells is found in the
bone marrow, blood or other lymph nodes that have size 0.2 mm or smaller.
M1: Evidences
have reveal the metastasis to another part of the body which means that breast
cancer cells are growing in other organs.
Cancer stage grouping
Doctors
have assigned the stage of the cancer by combination of T, N, and M
classifications and the grade of tumor and the results of PR/ER and HER2
testing. This information is used in determining the prognosis. T, N and M
classification is the simple approach for explaining the stages of cancer.
Different stages are described below on the basis of this approach.
The exact
stage of cancer is finalized after surgery usually about 5 to 7 days after
surgery. Doctor may termed stage I to stage IIA cancer as early stage cancer
and stage IIB to III as locally advanced cancer.
Stage 0: When the disease is only in the ducts of breast tissue and has not proliferate to the surrounding tissue of the breast. It also termed as noninvasive cancer.
Stage IA: The tumor is invasive, small and has not proliferate to the lymph nodes.
Stage IB: Cancer has proliferate to the lymph nodes
having size larger than 0.2 mm but smaller than 2 mm in size. There are no
evidences of tumor in the breast having size 20 mm or smaller.
Stage IIA: Any
1 of these conditions:
·
The cancer has proliferate to 1 to 3 axillary lymph nodes but
there are no evidences of tumor in the breast. It has not proliferate to the
distant parts of the body.
·
The size of tumor is 20 mm or smaller and has proliferate the
axillary lymph nodes.
·
The size of tumor is larger than 20 mm but smaller than 50 mm and
has not proliferate to the axillary lymph nodes.
Stage IIB: Either
of these conditions:
·
The size of tumor is larger than 20 mm but smaller than 50 mm and
has proliferate to 1 to 3 axillary lymph nodes.
·
The size of tumor is larger than 50 mm but has not proliferate to
the axillary lymph nodes.







